The Protest Psychosis & the Future of Equity & Diversity Efforts in American Psychiatry
This essay chronicles the history of medical associations between schizophrenia and Blackness that emerged during the tumultuous decades of the 1960s and 1970s, when American psychiatrists overdiagnosed schizophrenia in Black men in ways that undermined brain science of the era. I provide data to show how racially disparate diagnostic outcomes resulted not solely from the attitudes or biases of clinicians, but from a series of larger political and social determinants, most notably changing frameworks surrounding mental illness and political protest. I conclude by highlighting how training clinicians to examine their own cultural biases also needs to include training in how structures and institutions produce symptoms and diseases, and how we can only build better structures to support health if we can individually and then communally imagine them.
A worrisome trend emerged in the pages of leading medical and psychiatric journals during the height of civil rights–era America: psychiatrists were overdiagnosing schizophrenia in Black Americans at alarming rates. An extensive 1969 review of diagnostic patterns by the National Institute of Mental Health found that “blacks have a 65% higher rate of schizophrenia than whites.” Several years later, a series of articles published in the Archives of General Psychiatry uncovered how Black patients were “significantly more likely” than white patients to receive schizophrenia diagnoses and “significantly less likely” than white patients to receive depression diagnoses. Subsequent studies would find that Black men with schizophrenia were more likely to be hospitalized and receive higher doses of antipsychotic medications than were other persons with the illness.1
Were Black Americans prone to developing serious mental illness? Did psychosis spread among low-income populations like a virus, as sociologist R. E. L. Faris had shamefully argued?2
As is well known by anyone who trained as a psychiatrist after the 1960s, the psychiatric and medical establishments determined that race-based overdiagnosis was largely a social artifact brought to the clinical encounter by the arbiters of diagnosis: clinicians. Clinicians were applying “white norms” or outright racism, it was argued, onto their interpretations of Black minds.3
In response, any number of interventions emerged to teach health care providers to be less overtly or implicitly racist in their interactions with patients. By the time I trained in psychiatry some decades later, we learned to approach clinical encounters through frameworks of “cultural competency,” “interviewer honesty,” or through “standardized” diagnostic encounters that aimed to help clinicians better communicate with patients of diverse racial and ethnic backgrounds in ways that would improve communication and reduce disparities.
Mental health organizations then developed and promoted cultural “standards” for providers.4 I vividly recall mandatory modules that imparted ways to better understand how persons of “different” backgrounds expressed symptoms differently. The psychiatry department of a nearby hospital meanwhile opened a Black Focus Unit, complete with clinicians of color, African art, and, as reported in The Washington Post, “pictures of Vanessa Williams, Maya Angelou and Oprah Winfrey” on the walls.5
Though debatable by present-day standards, these efforts filled a gap that today seems almost unconceivable: before the 1960s, race was rarely a category of comparative analysis in psychiatric research, let alone an accepted topic of clinical dialogue.6
However, strategies that aimed to address clinician bias suffered from an important limitation: they often didn’t work. After decades of intervention, the overdiagnosis of schizophrenia in Black Americans, and related underdiagnosis of depression, anxiety, and a host of other conditions, remained largely unchanged. Nearly forty years after the National Institute of Mental Health study, an extensive 2005 analysis of psychiatric patient charts found that doctors diagnosed schizophrenia in African American patients, and particularly African American men, four times as often as in white patients, even though the research team uncovered no evidence that “black patients were any sicker than whites,” or that patients in either group were more likely to suffer from drug addiction, poverty, depression, or a host of other variables.7 A 2014 review of empirical literature on racial disparities in rates of psychotic disorder diagnoses found “a clear and pervasive pattern wherein African American/Black consumers show a rate of on average three to four higher than Euro-American/White consumers.”8 A 2018 meta-analysis found practically the same results.9
What had gone wrong?
As American medicine continues to grapple with the aftereffects of the murder of George Floyd, reckonings with unequal systems of justice, opportunity, and well-being that followed, and conservative backlash against “woke” education, I have been thinking anew about these civil rights–era findings, and the uneven psychiatric responses to them. Much like in the 1960s, 2020s-era protests led to charged assumptions about race, violence, and insanity.10 As in the 1960s, the implications of remonstrations about inequity reverberated through health care systems. And like the 1960s, after a series of machinations about seismic change, the response by these health systems focused centrally on changing clinicians’ attitudes, beliefs, and practices by “increasing awareness of inequities and discourse on the experience of oppression.” Psychologist Katherine Lingras and colleagues described a “reawakening to the importance of Diversity, Equity, and Inclusion (DEI)” happening at “Academic Health Centers . . . across the nation.”11
Such work remains vital, in large part because progress in matters of health equity occurs in fits and starts. The very notion that medicine and psychiatry require “reawakening” to the effects of injustice highlights the amnesiac nature of progress when institutions and providers are pressured to change.
At the same time, if increasing “awareness” remains at the center of 2020s-era efforts to address bias in health care, we risk forgetting the lesson of race-based misdiagnosis in the 1960s and 1970s: that beliefs and attitudes of providers, though vital to clinical communication, are largely immaterial to addressing systemwide disparities in health outcomes. That is because clinical encounters are often indicative of a host of upstream economic, social, ideological, and political structures that produce and racialize inequalities in health long before patients and providers enter exam rooms.
Consider race-based misdiagnosis. Around the world, worrying trends that emerged in the 1960s appeared indicative of extraclinical bias brought to the exam room—and in many instances, this was surely the case. But often lost on efforts to address race-based misdiagnosis of schizophrenia was the larger, structural fact that, for decades, schizophrenia coded as a “white” illness before it became a “Black” one.
Schizophrenia was coined by Swiss psychiatrist Paul Eugen Bleuler in 1911. Bleuler had cast schizophrenia as a “loosening of associations,” a process in which patients existed in the real world and at the same time turned away from reality (“autism”) into the world of fantasy, wishes, fears, and symbols. An early proponent of Freud, Bleuler defined schizophrenia as a psychical splitting of the basic functions of the personality, and believed that emotional splitting was accompanied not by violence, but by symptoms such as indifference, creativity, and passion.12
Given these origins, it is far from surprising that schizophrenia was applied in popular and psychiatric literatures to docile white housewives or ethereal white men of genius when the term entered American popular and medical discourse in the 1920s, 1930s, and 1940s.13 Publications like The New York Times described how white poets and novelists demonstrated a symptom called “grandiloquence,” a propensity toward flowery prose believed to be one of “the telltale phrases of schizophrenia, the mild form of insanity known as split personality.”14 Popular articles described middle-class women driven to insanity by the dual pressures of housework and motherhood. “Are we all going quietly mad?” asked an article in Better Homes and Gardens titled “Don’t Tell Them We’re All Going Crazy.”15 “Are you neurotic now? And if you are, does it mean that tomorrow you’ll be psychotic or schizophrenic?” According to an article from Ladies’ Home Journal titled “Are You Likely To Be A Happily Married Woman?” women suffered “schizophrenic mood swings” suggestive of “Doctor Jekyll and Mrs. Hyde.”16 Books like Mary Jane Ward’s autobiographical novel The Snake Pit similarly told stories of married white women driven to schizophrenia by the pressures of matrimonial life.17 Meanwhile, in clinical settings between the 1920s and 1950s, clinicians found schizophrenia disproportionally not in Black men, but in white women.18
The reasons schizophrenia coded as a white illness—and why it would later transform to a diagnosis that captured Black men—had relatively little to do with the actions of individual journalists, novelists, or psychiatrists. Rather, larger ideologies and economies undergirded these trends.
Frameworks of nosology were one important factor, inasmuch as for most of the first half of the twentieth century, psychoanalysis functioned as the dominant paradigm in American psychiatry. Psychoanalysis famously introduced American culture to neurosis, a set of symptoms that rendered white, middle-class women unable to fulfill their roles as mothers and as housewives. Schizophrenia was initially taken up by psychoanalytic authors who were more concerned with white minds than with Black bodies. Psychiatric journals, textbooks, and published abstracts frequently defined schizophrenia as a form of “emotional disharmony” that negatively impacted white people’s abilities to “think and feel.” Many psychiatric authors further assumed that “even the most regressed” patients with schizophrenia were nonthreatening and were therefore to be psychotherapeutically nurtured by their doctors, as if unruly children.19
Psychiatrists frequently highlighted Bleuler’s insistence that schizophrenia was an illness of personality. For instance, in the 1927 edition of his influential Textbook of Psychiatry, psychiatrist Arthur P. Noyes described schizophrenia as a rupture in “the fundamental basis of personality” that resulted in a disorder of “feeling and thinking.” Noyes wrote that persons prone to schizophrenia included “sensitive” persons who maintained “child-like facial expressions far past the usual age—an expression of vagueness and dreaminess.”20 The first and second editions of his textbook (1927/1936) used psychoanalytic language to explain how the ultimate cause of the illness was “intrapsychic conflict” that “weakened the forces of sublimation or of repression,” leading to disorders of the “emotions.”21
Similarly, the 1918 edition of the National Committee for Mental Hygiene’s Statistical Manual for the Use of Institutions for the Insane detailed how schizophrenia “afflicts . . . the seclusive type of personality or one showing other evidences of abnormality in the development of instincts or feelings.”22 Similar language appeared in many, though by no means all, scientific articles about schizophrenia throughout the 1920s, 1930s, and 1940s. Psychoanalyst Otto Fenichel, among others, described schizophrenia as a “special kind of neurosis” amenable to psychoanalytic talk therapies.23 As late as 1952, the first postwar classification of psychopathology, Diagnostic and Statistical Manual: Mental Disorders (later known as DSM-I), similarly emphasized that schizophrenia was a “nonorganic” condition that represented underlying psychological conflicts or maladaptive reactions to life stressors.24
Clinicians were of course free to diagnose mental illness as they saw fit. But the framing of schizophrenia over the first half of the twentieth century clearly reflected existing ideas about white minds, relationships, and civilizations, and thereby marked schizophrenia as a disease of the white mainstream in ways that encouraged identification with certain groups of persons while rendering other groups invisible. The framing of the illness encouraged psychiatrists to locate the illness in the types of patients who could afford therapy, or the kinds of patients that hospitalists or researchers saw in America before desegregation on “whites-only” wards of psychiatric hospitals. Such strategies meanwhile occluded recognition of the countless men and women who resided in so-called Negro Hospitals and suffered well outside most realms of public awareness.25
In my book The Protest Psychosis, I detail the totality of schizophrenia’s racial shift between the late 1950s and the present day.26 This racial transformation began, not coincidentally, as psychiatric hospital wards desegregated and as expanded community mental health clinics put mental health providers into contact with “community” patients.
During this time, a growing body of research emerged suggesting that, while shaped by developmental and environmental confounders, mental illnesses like schizophrenia ultimately resulted from aberrations of brain biology. The promise of biological psychiatry was that it would obviate the gender biases wrought by psychoanalysis. Moreover, because the potential biological substrate for the illness occurred far beneath the skin and its various pigmentations, the logic implied, schizophrenia should occur in all peoples and all places equally.
Of course, that’s not what happened. Starting in the 1960s, not only was the diagnosis increasingly located in Black Americans in general, and Black men in specific, but the reframing of the illness cast many people previously seen as schizophrenic, such as white women, into diagnoses that included depression, anxiety, and various personality disorders.
My analysis in The Protest Psychosis focuses on how upstream factors reframed schizophrenia in ways that encouraged psychiatrists, the medical system, and white mainstream American society to “see” Black men as schizophrenic, and treat them as such. A key part of my argument focuses on how, in 1968, in the midst of a political climate marked by political protest, psychiatry published the second edition of the Diagnostic and Statistical Manual. That text recast the paranoid subtype of schizophrenia as a disorder of masculinized belligerence. “The patient’s attitude is frequently hostile and aggressive,” DSM-II read, “and his behavior tends to be consistent with his delusions.”27
I show how growing numbers of researchers used DSM-II criteria to conflate schizophrenia diagnoses in Black patients with Black political protests. The title of the book came from a 1968 article in the Archives of General Psychiatry by two psychiatrists, Walter Bromberg and Franck Simon, who described a condition in which the rhetoric of the Black Power movement drove “Negro men” to insanity marked by violent delusions, anger, hostility, and projection (“The delusions are clearly paranoid projections of racial antagonism of the Negroes to the Caucasian group”).28
Similarly, in an article titled “Six Years of Sit-Ins: Psychodynamic Causes and Effects,” psychiatrists Chester Pierce and Louis Jolyon West argued that “Negroes” developed delusions, grandiosity, magical thinking, and “dangerous aggressive feelings” when they participated in civil-rights sit-ins (Pierce was a distinguished African American psychiatrist).29 Psychiatrists Allen Raskin, Thomas H. Crook, and Kenneth D. Herman wrote that “blacks” with schizophrenia rated higher than “whites” on a set of “hostility variables” due to delusional beliefs that “their civil rights were being compromised or violated.”30 In a series of high-profile articles titled “Social Conflict and Schizophrenic Behavior in Young Adult Negro Males,” social psychiatrist Eugene B. Brody argued that “black culture” was itself a risk factor for schizophrenia. Here and elsewhere, civil rights–era themes of liberation were recast as symptoms of mental illness.31
I now realize that, if anything, I understated the problem. In the years since the publication of The Protest Psychosis, I have continued to track the shifting associations between schizophrenia and race to help explain why overdiagnosis of Black men persisted even after psychiatry changed the language in the DSM, implemented cultural-competency training, and put in place a host of other interventions meant to assure that all persons were diagnosed and treated equally. Through my continued work, I have begun to understand that changing the diagnostic codes and clinician attitudes was not enough because, in the 1960s, the structures undergirding language, observation, and clinical common sense, and the institutions we built to reflect them, also shifted.
For instance, with two colleagues—Sara McClelland and Erin Bergner—I have dug deeper into the racial assumptions surrounding ways that researchers described patients with schizophrenia in the decades leading up to and then following DSM-II. Over several years, we systematically pulled general/random articles about persons with schizophrenia published in leading psychiatric journals between 1949 and 1980 (that is, American Journal of Psychiatry, Archives of General Psychiatry, American Journal of Orthopsychiatry, and Psychiatry) against articles about schizophrenia from the same period that specifically mentioned the race of patients with the illness. We first searched the databases OLDMEDLINE and MEDLINE for articles that included the term schizophrenia in their titles or abstracts, and then performed the same search for articles that mentioned schizophrenia in their titles or abstracts alongside terms that connoted racially, geographically, or ethnically distinct populations or forms of schizophrenic illness. These terms were culled from a larger, extensive survey of race and what were in the 1950s called “nativity” categories historically deployed in U.S. medical literature, including “Caucasian,” “white,” “Negro,” “colored,” “black,” “African American,” “Mexican,” “Italian,” “Jew/Jewish,” and “Oriental.”32 These searches yielded thousands of articles, which we then reduced by stratified random sampling, followed by content coding.33
Our first realization from this simple analysis was that, even before random sampling, there were nowhere near enough race and ethnicity descriptors for comparison, with one notable exception. The terms “white” and “Caucasian” yielded inconsistent results (some of which referenced nonracial color; for example, “white blood cells”), and authors did not always specify the racial demographics of their samples, except in the cases when the samples were exceptional (but these terms lacked specificity, such as “non-white”), leaving only thirty-nine articles over a four-decade span that isolated white patients expressly. Only fourteen articles discussed schizophrenia in relation to non–African American “ethnic” populations (for example, “Mexican,” “Irish,” “Jews”). But 737 articles expressly described patients with schizophrenia as “Negro,” “colored,” “black,” or “African American.” This led us to surmise that many of the random/general articles about schizophrenia (n=1,468) assumed whiteness as a norm, while almost all test/race articles assumed deviance from that norm as Blackness.
Similar to the random/general sample, we next reduced the test/race dataset by stratified random sampling and began content coding. We first quantified the most frequently used descriptors in each time period.34 The random/general articles described patients as being largely passive and withdrawn, as seen in Table 1. As expected, the test/race articles emphasized aggressive actions, as seen in Table 2.
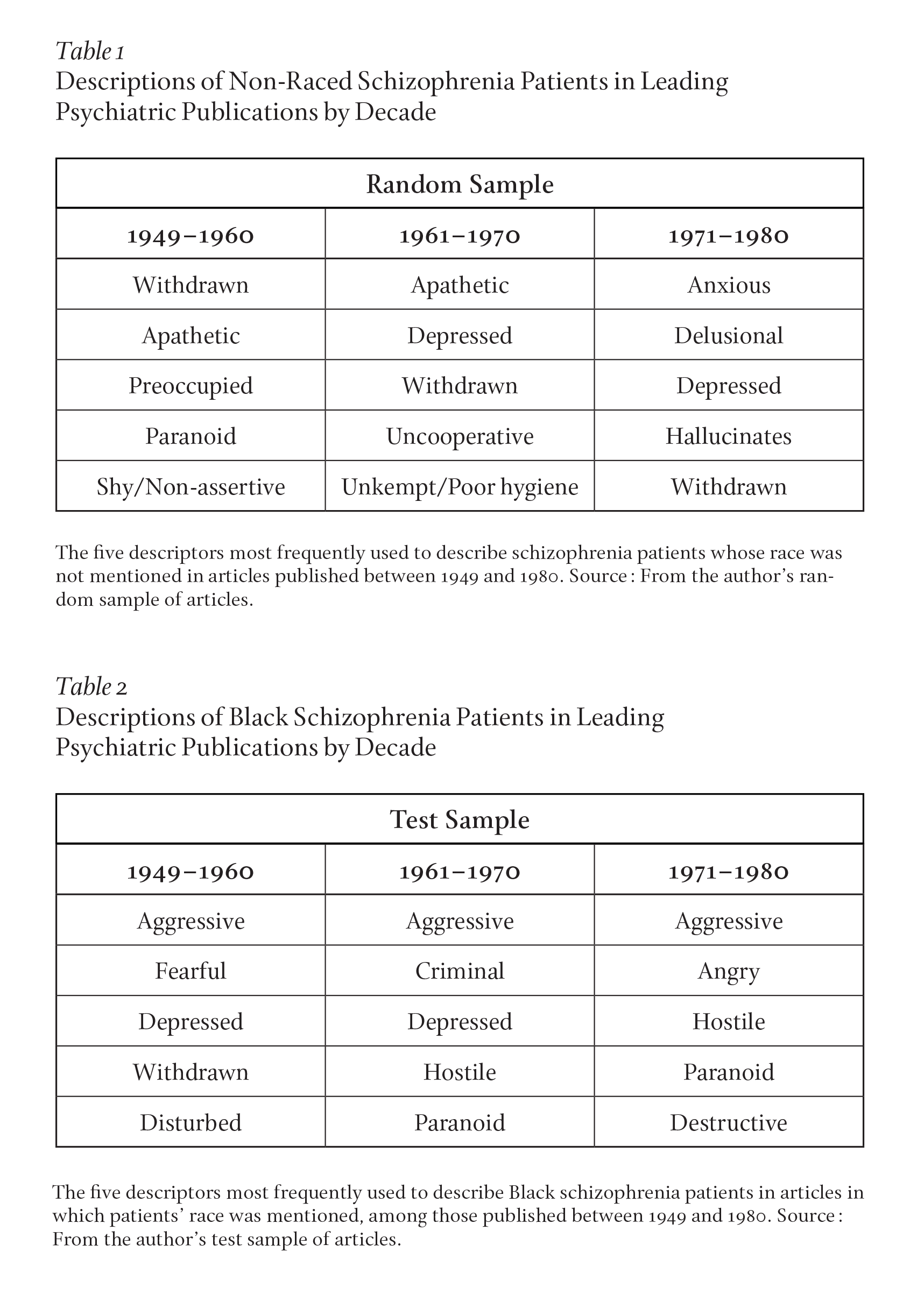
Black men with schizophrenia were often described in clinical and scientific literature not as docile or wandering, but as threatening and in need of containment rather than enlightenment. These findings suggested that DSM-II indeed provided language to pathologize Black political protest and “aggression” in the 1960s. But it also showed that such associations gave way to other racially charged terms and observations even after much of the problematic terminology in DSM-II was removed from the subsequent DSM-III in 1974.
Relatedly, we found that while authors of random articles justified diagnoses through symptoms that altered emotions or personalities, writers of test/race articles increasingly justified illness by highlighting pathological behaviors (p=0.05). Figure 1 shows the split between four aspects these authors used as diagnostic tools.
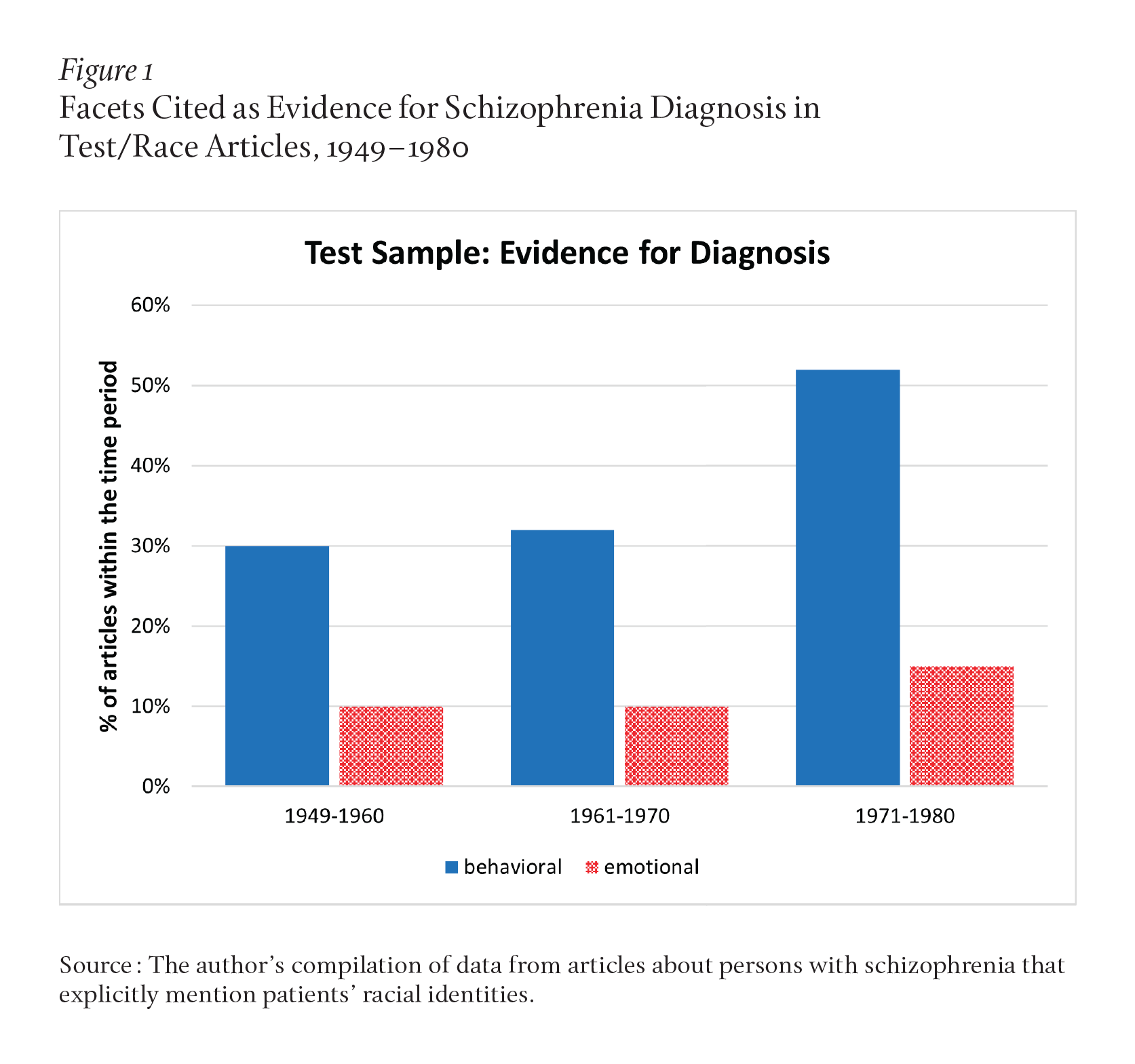
To be sure, 21 percent of the random/general articles mentioned behaviors, and often these behaviors were construed as aggressive. Even then, such actions were rarely if ever linked to deviance. By contrast, aggression by patients described in the test/race sample was routinely linked to criminal and illegal behavior, while authors of articles in the random sample made no such connections at all.
Examples from our growing database, which will serve as the foundation for a follow-up volume that extends the analysis from The Protest Psychosis to the present day, often connected family or developmental history to intellectual or cognitive decline. For instance, an article about schizophrenia from 1955 explained how “a patient with such a profile would be expected to have a thinking disorder and to be anxious, apprehensive and dysphoric.”35 Articles in the random sample also frequently emphasized social isolation, poor hygiene habits, and affective or emotional withdrawal in persons with schizophrenia. A study design from 1961 explained how “Each hospital prepared a list of 40 apathetic, withdrawn, but physically healthy schizophrenic men.”36 And from a 1978 article: “Severely disabled schizophrenic patients with little capacity for spontaneous communication were left to their own devices and spent a very large proportion of their waking day doing absolutely nothing. They became very much more withdrawn and underactive and apathetic.”37
Again, hostility appeared in select articles in the random sample, but such articles never presented aggression in ways that implied threats to doctors or to society at large. Moreover, articles in this frequently race-neutral sample never connected aggression to larger group characteristics based on race, social class, or political orientation. For instance, a 1968 article described a male patient—“his behavior is unremarkable; affect is generally apathetic, but he displays flashes of hostility”—as being calmed by talk therapy, sedatives, and “simple gardening chores.”38 By contrast, authors described test-sample subjects as aggressive, hostile, and threatening in a number of more ominous ways. Terms and phrases that implied criminal intent appeared through the sample with increasing frequency over time. A 1972 article contended that Black patients with schizophrenia “were openly hostile and saw their hospitalization as representative of the treatment generally afforded blacks by the white society.”39 Researchers in 1969 asserted that “it is clear that rapid shifts in the social milieu of the Negro are shifting the concerns about adequacy in regard to power to an assertive posture.”40 Test sample articles also frequently used DSM-II language to emphasize behavioral symptoms over cognitive or intellectual ones. Authors of a 1975 study wrote that, “Black males rated themselves significantly higher than the other groups on the Outspokenness and Assault factors. . . . Both of these factors share in common the impulse to strike back, either verbally or physically, when an individual feels his rights are being violated.”41
Shifting linguistic trends over four decades in mid-twentieth-century literature suggest that overdiagnosis was more than a problem of diagnosis: It was a problem that reflected broader associations built into observations and descriptions. Casting Black men as violent made “sense” in the context of an era of political unrest, and these associations remained embedded in the frameworks surrounding diagnostic observations after the moment of conflict passed and the diagnostic language changed.
Observations and descriptions in turn validated interventions—inasmuch as, if mental illness were seen as a disorder of bodily threat rather than of personality, it would follow that such bodies would be treated with ever-more-tranquilizing medications. In an endless feedback loop, bodily racial schizophrenia was seen as potentially criminal, which paved the way for institutions that justified bodily control, made manifest by growing associations between psychiatry and the prison industrial complex. Mental hospitals closed, and prisons emerged as underfunded, understaffed “pseudo mental hospitals.”42
Perhaps at the beginning of the process, associations between schizophrenia, race, and violence made sense to diagnosing clinicians. But after decades—and certainly by the early twenty-first century, when the number of persons diagnosed with schizophrenia who reside in prisons far surpasses those in psychiatric care facilities—we are left standing outside the walls of the institution wondering how in the world things got to be this way, and what on earth might be done to change them.43
What can be gleaned, then, by the racial transformation of a diagnosis?
Undoubtedly, some of the clinicians who diagnosed unjustly, much like authors of articles that described Black men with protest psychoses, were racist. And in this sense, this represents yet another case study in the annals of medical racism.
But a key lesson of history is that the race-based overdiagnosis of schizophrenia in Black men was as much a consequence as it was a symptom of larger structural ills. In a broader sense, overdiagnosis ultimately resulted not solely from the attitudes or biases of clinicians, but from a series of larger political and social determinants.44 The official psychiatric diagnosis of schizophrenia changed. Anti-psychotic medications altered the focus of psychiatric treatment from talk therapies that promoted insight to medication-induced sedation and corporeal control. The function of psychiatric institutions themselves then shifted ever closer to keeping patients deemed “dangerous to others” out of society. Even the most self-aware, empathic, and culturally competent clinicians functioned within a larger system that aligned Blackness with insanity. Black men became schizophrenic as a result of these transformations.
No doubt, the language in many of these articles I have cited would be deemed unacceptable in the present day, thanks in no small part to interventions like cultural competence and DEI training. But that is in part the point: if we better understand the mechanisms that allowed problematic assumptions of the past to be at the time so acceptable that they found audience in top tier journals, we must then consider which assumptions that seem sensical or commonplace today will yield disparities in the future.
Of course, people build structures and institutions. Structures and institutions in turn reflect amalgams of individual values and decisions. Calling bias “structural” in no way implies that individuals be given a free pass. To the contrary, we can only build better, more equitable structures if we can individually and then communally imagine them.
Many scholars, myself included, have thus begun to address racism through a framework of “structural competency” to highlight ways that training clinicians to examine their own cultural biases insufficiently addresses inequity without training them to also understand how structures and institutions produce symptoms and diseases. Structural competency builds on Stokely Carmichael’s notion of “institutional racism” to promote reforms that push back against the increasing connectedness of psychiatry and the prison industrial complex, critically addressing multiple aspects of medical education, clinical practice, and health care delivery systems more broadly.45
Another lesson of history is that moments of racial reckoning and protest, from the civil rights era to the protests after George Floyd’s murder, present and foreclose opportunities to address health justice. Protests raise the specter of new coalitions that confront seemingly intractable social problems. Solutions can in turn move people closer to building what economist Amartya Sen calls “better societies.” Here, moments of peril or unrest spark appreciation of shared humanity and renew drives toward building shared and mutually beneficial infrastructures that persist well after the crisis has subsided. National health care systems, for instance. Or expanded and affordable mental health clinics. Or reformed police, protected climates, or effective infrastructures and food distribution networks. As Sen explains it, societies that react to moments of crisis by democratizing access to resources, health, and decision-making power come out ahead in the long run.46
We learn this lesson time and again: equity can improve life and livelihood for everyone. Better community mental health reduces the burden on overwhelmed mental health systems. Fair policing and safer neighborhoods improve the vitality of cities.47 Addressing the inequities that rendered disadvantaged communities more vulnerable to COVID-19 better prepares states to face future pandemics.48 Closing the racial wealth gap—and allowing more people to access education, employment, consumption, and investment—boosts the U.S. national GDP by 4 to 6 percent.49 And on and on.
Then there is the inevitable other response to social justice movements, the one we see in misdiagnosis. The reflexively defensive response that frames the world through what political theorist Heather McGhee devastatingly describes as “zero-sum” thinking, in which there can be only winners or losers in fights for mental health.50 Such responses provoke not solutions to complex problems, but structural reifications of their underlying pathogenic assumptions.51
Civil rights protests represented important points along that continuum. Calls for fair treatment and access—indeed, the era saw the rise of the community mental health movement and health clinics run by the Black Panthers—were met with support among many people and profound resentment among others. Resistance to change emerged in high-profile public sites like schools and lunch counters. And it occurred in countless other invisiblized places like private conversations, everyday interactions, and frameworks that guided diagnostic knowledge and common sense.
Ultimately, history leads us to ask: what enduring accomplishments will come from present efforts to address health equity and justice? And what will serve as this moment’s invisible, enduring obstructions? No doubt, language matters in all things, and particularly so in clinical interactions. Patients describe symptoms, clinicians listen and ask for elaboration, and together they make effective treatment decisions. Language also shapes the ways that clinicians understand, classify, and manage illnesses.
But a final lesson of history is that calling out and changing problematic language is not enough. When clinical language is found to be racist, replacing it with more acceptable phrasing does little to change outcomes if not combined with attention to the larger structures that produce its inequities in the first place. Including, it would seem, the very frameworks through which we diagnose illness and aim to restore health.